
Intuitive interface and solution flexibility reduce the time and costs of the insurance claim handling process.
Comarch Insurance Claims is an innovative and comprehensive claims management software for life and health insurance companies. The system supports claim handling processes end-to-end, from registration and calculation to decision-making and benefit payment, accelerating the everyday work of the claim manager. This claims management system meets the most important requirements of insurance companies operating in the rapidly growing market.
Software designed for insurance companies

Smooth information flow, automated processes, and optimization of monitoring of the claim processes
Shorter time needed for claim handling, optimized operating costs
Automated internal and external payments, along with calculation of benefits, automated verifications and calculations
Validation rules supporting effective decision-making and limit control
Boost the quality of customer services through quick decisions and payments
Better process monitoring, data integrity and a single source of truth
Standard functionalities available in all Comarch claims management systems to support insurers’ companies:
The Comarch Insurance Claims system covers the whole claim process, from registration through verification and decision-making to payment and document dispatching.
Specific claim stages and functions are:

All liabilities arising from claim handling should be paid seamlessly.
The Comarch Insurance Claims system provides:

The claims software handles document generation, triggered automatically or manually by the user on-demand, and supports other functions connected with documents:

More advanced functions provide:

Comarch Insurance Claims supports all areas of claims handling. One of the main goals of our claims management software is to automate the full claim process, reducing its time and costs. The claims system supports insurance companies in gaining a competitive edge thanks to quick benefit payments, professional customer service, and easy configurations of claim processes.
Features of the Comarch Insurance Claims system are:
Integrate Comarch Insurance Claims with Comarch Digital Insurance – an omnichannel system for front-office departments. Create one process for distributors, customers and claims managers end-to-end.
With Comarch claims processing systems, you will create a single environment in which claims are reported by distributors, call center operators, or directly by end customers and then automatically sent to the system for claims handling. Allow all process participants to go through it smoothly and check the current process status. Additional documents required during the process will be delivered faster and easier.
Read more about Comarch Digital Insurance and its benefits:

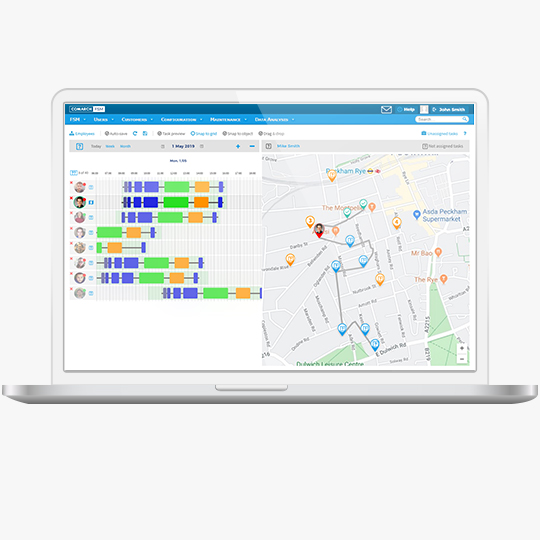
Comarch FSM – software and mobile app for claims adjustment
Automate claims assignment, routing, gathering documentation, reporting and auditing with advanced features.
Tell us about your business needs. We will find the perfect solution.